Major Principles
Major Principles
1
Before doing a buckle, it is critical to perform a detailed and accurate scleral depressed exam to identify all of the retinal breaks and relevant pathology.
2
Relieve vitreoretinal traction on the breaks and relevant pathology by placement of an appropriate buckle element
3
Treat the breaks (cryotherapy, or laser subsequently when retina is flat)
Which Buckle
Which Buckle | Types of Scleral Buckles
-
1. Circumferential encircling buckle
A buckle element that wraps around the entire circumference of the eye and achieves height by tightening of the buckle (like a belt). E.g. #40, #41, #240
-
2. Segmental circumferential element
A buckle element that is placed in only one segment of the eye to cover the relevant pathology in that region and oriented circumferentially. Height is achieved by imbrication of the sutures. E.g. 506, 511, 276, 220, etc. Some of these are grooved (of which many end in “G”) to enable placement of an encircling element into the grove.
-
3. Segmental radial element
A buckle element that is oriented radial to the limbus. Height is achieved by imbrication of the sutures. These achieve shortening of the eye without shortening of the retina and thus reduce development of retinal folds. In addition there are radial wedges that can be placed radially under an encircling element (E.g. #135, #137)
-
4. A combination of the above
Which Buckle | Selecting the Right Buckle
A variety of buckle elements can effectively treat a given retinal detachment. The specific buckle used is often surgeon-specific. As a general principle, the breaks should all be well supported on the buckle element and the smallest buckle element or combination of buckle elements that support the pathology should be utilized in order to minimize morbidity from the buckle.
Scleral Buckling Technique
Scleral Buckling Technique | Exposure
-
1. Exposure
Conjunctival peritomy, usually 360 degrees (forcep and Wescott scissors).
Less extensive peritomy can be performed for segmental buckles to provide exposure to the buckled quadrants and muscles that will need to be isolated to torque the eye for exposure.
Take care to avoid conjunctival buttonholes that can risk buckle exposures and to cleanly dissect Tenon’s capsule.
Creating a limbal peritomy
Creating a peritomy
Isolation of the 4 rectus muscles (2-0 silk suture and Gass retinal detachment hook; some surgeons first use the Jameson hook to isolate the muscle first). For segmental buckles, only a subset of the muscles may be isolated, rather than all 4. After isolating the muscle and before tying a knot in the 2-0 silk, the muscle insertion should be inspected to confirm that the muscle has been isolated in entirety (not split). If the muscle has been split, remove the suture and re-isolate the muscle.
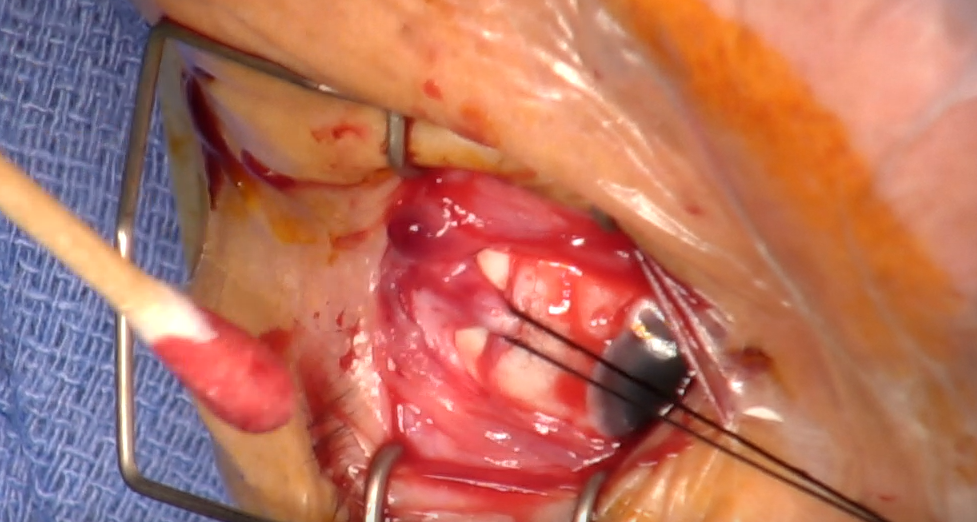
Dissection of the oblique quadrants and isolation of rectus muscles
Clearance of Tenon’s from the isolated muscles (Wescott scissors and/or sterile swab). Be wary of the levator muscle fibers when working over the superior rectus. Some surgeons advocate not performing this over the superior rectus or only carefully using a swab.
Using the Schepen’s retractor, the sclera should be inspected in all 4 quadrants to identify any areas of thinning and/or prominent or anomalous vortex veins, both of which pose a risk for perforation during suture passes.
Scleral buckling technique
Scleral Buckling Technique | Marking the retinal break(s)
Use an indirect ophthalmoscope and a sterile 20 or 28D lens, with the room lights turned off. Use the 2-0 silk muscle sutures in one hand to move the globe and an O’Connor scleral depressor in the other hand and identify the retinal break.
When the break(s) is found, rotate the O’Connor depressor so the break is “marked” by the rounded Gass marker at the bulb of the depressor. This rim of metal at the end of the bulb, when applied to the sclera, dehydrates the sclera temporarily, leaving a dark black round mark. Turn on the room lights, expose the sclera to identify the round mark, and mark the spot using a marking pen.
Marking the retinal break(s)
A forcep can be used to gently hold the sclera at the site of the mark and then use it as a gentle depressor while viewing through the indirect ophthalmoscope to confirm that the mark is appropriately placed.
Repeat for any other breaks.
Scleral buckling technique
Scleral Buckling Technique | Treating the retinal break(s)
After marking, cryotherapy may be applied to the breaks. Care should be taken to sufficiently treat the breaks, especially the apices of horseshoe tears, but to avoid excessive cryotherapy.
Cryotherapy
Care should be taken to avoid “shafting” of the probe, in which the shaft, rather than the tip, is visualized during the depression and thus cryotherapy is applied far more posteriorly than intended.
Some surgeons do not perform cryotherapy but rather apply laser at a later date when the retina has flattened.
Scleral buckling technique
Scleral Buckling Technique | Placement of the buckle and sutures
The buckle is secured in the correct location (relative to the marked break(s)) via suture or belt loops.
- Suture options: 5-0 non-absorbable synthetic (e.g. 5-0 nylon or 5-0 mersilene)
- Needle: spatulated with cutting tip
- Type of suture pass: horizontal mattress suture
Safe suture pass technique: the field should be dry and largely free of blood. Tenon’s capsule should have been cleanly dissected to reveal bare sclera as additional tissue on the scleral surface renders it difficult to gauge depth of the suture pass accurately. The buckle should be moved out of the way if it has already been placed at the time of suture passes (e.g. encircling buckle). A partial thickness (1/2 or 2/3 thickness) scleral pass should be made of approximately 4mm in length. The pass should be performed slowly, and when removing the needle from the sclera, the curvature of the needle should be followed – i.e. care should be taken to avoid torquing the needle such that the hub can poke into the sclera and cause a perforation.
Segmental Buckles
For segmental buckle elements, in which height is attained by suture tightness and the length of the suture relative to the size of the buckle, imbrication is required to achieve height of the buckle. Thus, the distance between the two scleral passes comprising the mattress suture must be greater than the size of the buckle – usually 2-3 mm wider than the buckle width. For example, for a 516G grooved element, which is 6.4mm wide and 2.3mm high, the scleral passes may be placed approximately 8.5mm apart.
The suture passes are made parallel to the limbus for circumferential elements and tangential to the limbus for radial elements. Two horizontal mattress sutures are placed in each quadrant.
Calipers should be used to mark the distance between the suture bites (or passes), such that the mark signifying the retinal break(s) is in the center. Ideally, the buckle will support both the posterior-most aspect of the break and also the vitreous base.
Subretinal fluid drainage may be performed in the bed of the future buckle at this time, if needed (see below subretinal fluid drainage section). Drainage is best performed after placement of all sutures to avoid passing sutures in a soft globe, which risks perforation, and before placement of the buckle element, which (except for low profile encircling buckles) can crowd the surgical field and come out of position during manipulations for drainage.
The element is passed under the suture loops and relevant rectus muscles.
A variety of techniques can be used to tighten the sutures around the buckle element and ensure imbrication. For example, for sponges, the assistant can pull both ends of the sponge so the sponge is thinned. The surgeon then ties the knots. Alternatively, if subretinal fluid drainage was performed, the softness of the globe will result in imbrication with standard suturing technique over the buckle element.
Appropriate suture tying technique is also critical to achieve appropriate imbrication by not allowing the suture knot to loosen between ties. For example, the needle drivers should be used to grasp the suture close to the knot and the sutures lifted and flatted multiple times to tighten the suture. Undue force should not be applied as this is ineffective for suture tightening and risks suture breakage. In addition, after the first knot is placed, the assistant can hold the knot (to prevent its loosening) while the surgeon passes the subsequent knot.
Indirect ophthalmoscopy should be performed to visualize the buckle and to confirm that the optic disc is perfused. If it is not and/or the intraocular pressure if palpated to be high after buckle tightening, a 30g needle can be used for anterior segment paracentesis. Repeat ophthalmoscopy should be performed to confirm that the pressure was sufficiently reduced to reestablish perfusion of the optic disc. Repeat aqueous paracenteses may be required after the chamber refills.
At this point, some surgeons may administer an intraocular gas bubble (e.g. as an adjunct, especially for superior breaks or in the setting of subretinal hemorrhage related to suture passes or subretinal fluid drainage, or for superior breaks that may not be well positioned on the buckle). Anterior chamber paracentesis may need to be performed before or after placement of the gas bubble to create space/prevent severe intraocular pressure elevation.
Encircling Buckles
Instead of using sutures to secure an encircling buckle, the buckle can be placed under “scleral belt loops” – lamellar flaps of sclera. When using belt loops, the belt loops are created first, and the buckle passed underneath thereafter. For example, a crescent blade, guarded #57/#64 Beaver blade, or limbal relaxing incision diamond blade (approximately 250 micron depth) may be used to make radial scleral partial thickness incisions (approx. 3 mm apart and the length as determined by the width of the buckle). A Beaver blade can then be used to perform a lamellar dissection to connect the two radial incisions. The buckle is passed under the lamellar scleral flap like a belt loop. Preference regarding belt loops versus suturing are often surgeon-specific.
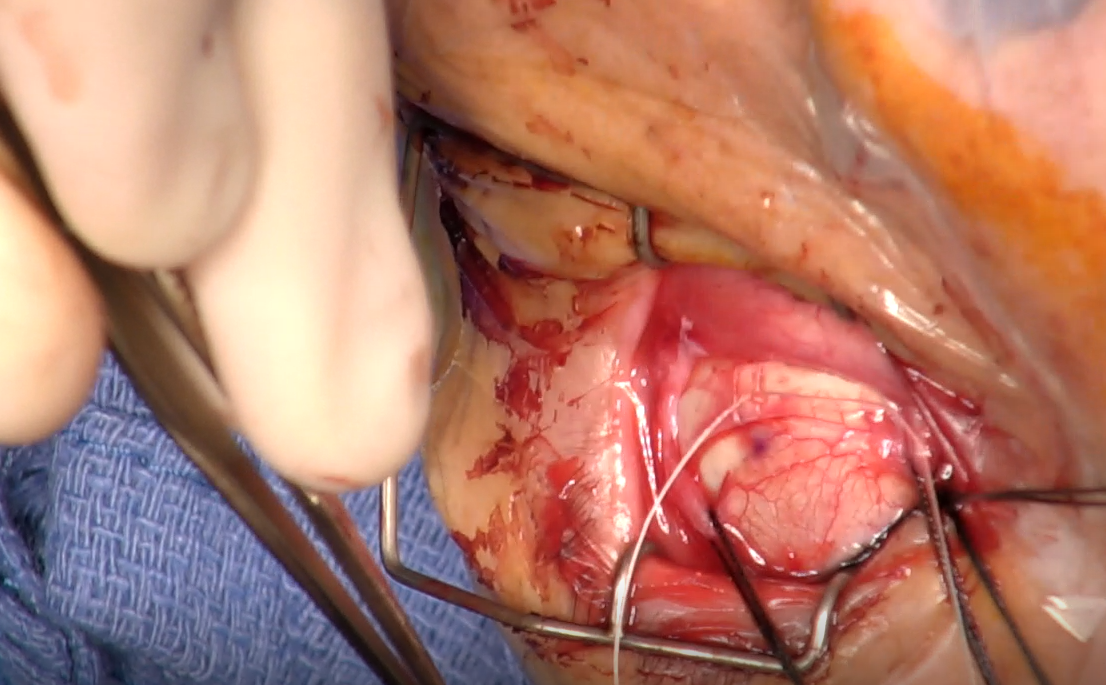
Securing the band with belt loops
When using sutures for encircling bands, the buckle is generally passed first, under the muscle insertions using Nugent forceps, taking care to ensure the buckle does not twist.
Passing the scleral buckle
A Watske or other sleeve (e.g. #70, #270) is placed to secure the buckle.
Placing the sleeve
Sutures are then placed, generally one horizontal mattress suture per quadrant. Suture tracks for encircling elements, in which height is achieved by circumferential tightening of the buckle like a belt, rather than the tightness of the sutures, may be a bit shorter and less deep than that required for segmental elements. Thus, the passes need not be long, deep, nor tight. Occasionally, if extra height is desired, imbrication may be performed as with elements. In general, the depth should be such that the gray of the needle is barely visible under the sclera at all times.
The suture passes are made parallel to the limbus.
When used to support breaks that were marked, the suture passes are made to straddle the mark. When used to support the vitreous base, the scleral passes are usually arranged such that the anterior pass lies approximately 3 mm posterior to the muscle insertions (or the imaginary line connecting the rectus muscle insertions). Usually, one horizontal mattress suture is placed in each quadrant.
Subretinal fluid drainage may be performed in the bed of the future buckle at this time, if needed (see below subretinal fluid drainage section). Drainage is best performed after placement of all sutures to avoid passing sutures in a soft globe, which risks perforation, and before tying of the sutures (to enable free movement of the buckle out of the way for manipulations for drainage).
The sutures are then tied. They need not be tied tight as the buckle achieves height through belt tightening, rather than imbrication. Occasionally, if an especially higher buckle is desired (e.g. in the area of a marked break), then imbrication may also be performed.
Indirect ophthalmoscopy should be performed to visualize the buckle and to confirm that the optic disc is perfused. If it is not and/or the intraocular pressure if palpated to be high after buckle tightening, a 30g needle can be used for anterior segment paracentesis. Repeat ophthalmoscopy should be performed to confirm that the pressure was sufficiently reduced to reestablish perfusion of the optic disc. Repeat aqueous paracenteses may be required after the chamber refills.
Indirect ophthalmoscopy also confirms position of the scleral buckle relative to the breaks. If it is noted that one or more breaks are posterior to the buckle, an additional sponge may be considered (or a radial sponge element) under the existing buckle to better support that pathology.
At this point, some surgeons may administer an intraocular gas bubble (e.g. as an adjunct, especially for superior breaks or in the setting of subretinal hemorrhage related to suture passes or subretinal fluid drainage). Anterior chamber paracentesis may need to be performed before or after placement of the gas bubble to create space/prevent severe intraocular pressure elevation.
Scleral buckling technique
Scleral Buckling Technique | Closure
After trimming the buckle, Tenon’s capsule may be closed first, separately from conjunctiva. This may reduce risk of buckle exposure and may be considered especially for sponges or large elements (vs. for low profile encircling buckles). 7-0 Vicryl suture can be used to grasp Tenon’s capsule alone and then anchor it to the fibrous tissue on either side of the muscle insertions.
Conjunctiva is reapproximated using 7-0 Vicryl suture or 6-0 Plain gut suture.
VBS Virtual Series 2020 Scleral Buckle Surgery Pearls
Other Techniques Related to Scleral Buckling
Other Techniques | Subretinal fluid drainage
When to drain
Some surgeons drain all or most subretinal fluids, whereas others almost never drain. In general, drainage is most indicated when necessary to allow the breaks in a very bullous detachment to settle on the buckle (reapposing the retina on the RPE and thus facilitating their closure postoperatively) or for chronic (often inferior) subretinal fluid. Drainage is least indicated for shallow detachments in which the break settles nicely onto the buckle without drainage or for more recent detachments (often superior). When subretinal fluid is not drained, the fluid will often slowly reabsorb, though progress can be very slow, depending on the chronicity of the fluid.
Drainage techniques
A variety of techniques may be employed (outlined below) but the basic premise is to achieve controlled entry into the subretinal space to allow egress of subretinal fluid, ideally in a location where the subretinal fluid is most bullous and under the bed of the buckle so that the area is supported in the event of a retinal perforation / break. Care should be taken to look for and avoid any vortex veins.
Drainage should be performed in an area of significant subretinal fluid after placement of sutures but before tying of the sutures. Encircling buckles may have been placed and can be moved out of the way but large buckle elements should not be placed until after drainage if possible.
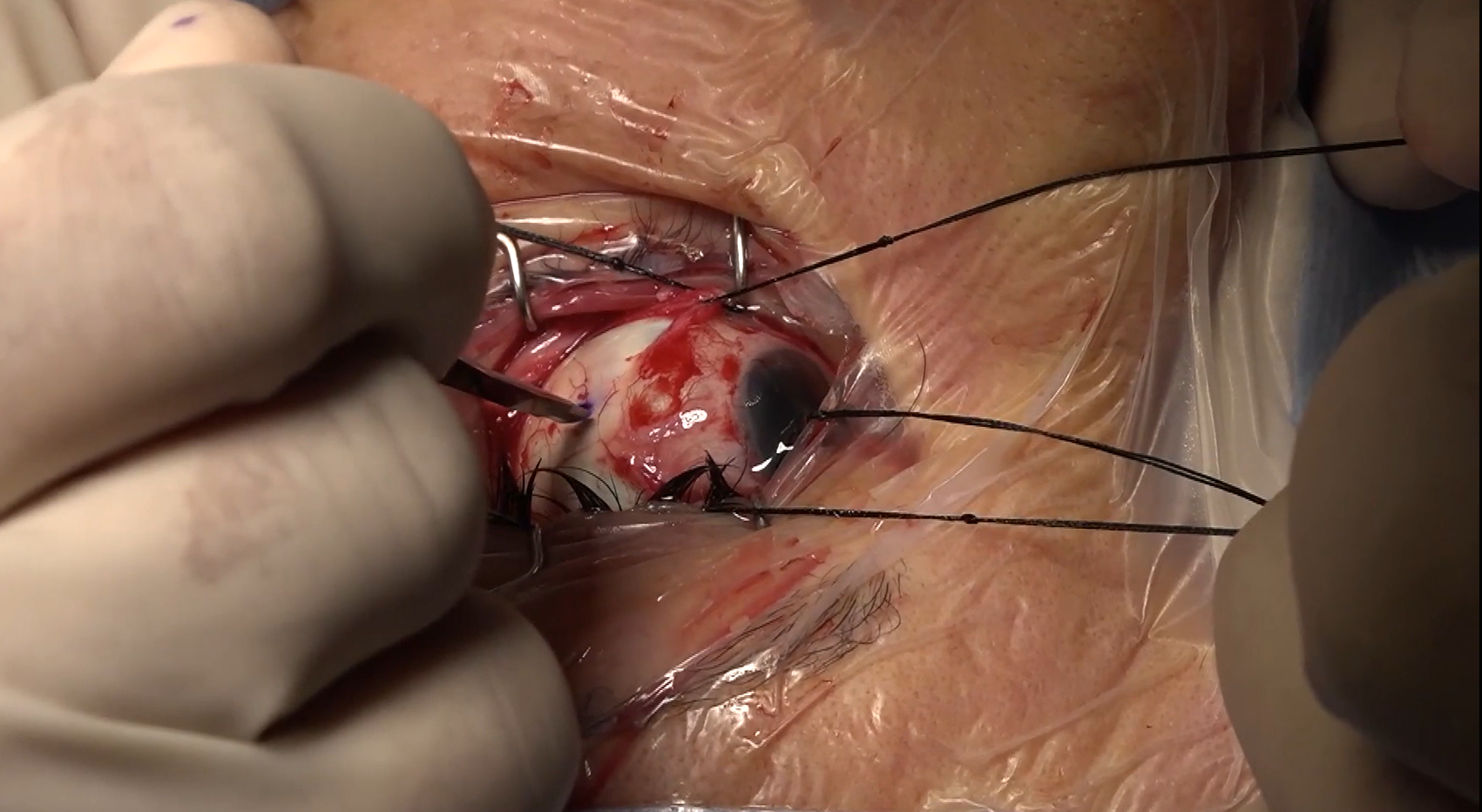
Small radial sclerotomy (2 mm) under the anticipated bed of the buckle. A Grieshaber blade or similar instrument is used to make serial incisions in the sclerotomy site to gradually deepen it until the blue of the choroid is identified. Diathermy may be applied to the edges of the sclerotomy. Tension on the 2-0 silk sutures on the muscles should be relaxed to avoid a highly pressurized globe at the time of entry into the subretinal space. A needle (26 - 30g hollow bore needle on a syringe with the plunger removed, with the bevel facing the sclera, or a tapered suture needle is inserted through the choroid into the subretinal space and clear or yellowish translucent fluid should egress. To control the depth of entry of the needle, it may be "guarded" – for example by placing the needle driver close to the tip of a tapered suture needle, or placing a buckle sleeve (#70 or #270) on the end of the hollow bore needle. Swabs may be placed into the fornices or tension reapplied on the 2-0 silk muscle traction sutures to increase the intraocular pressure and promote egress of subretinal fluid. Pigment granules may be noted in the egressing fluid towards the end of the fluid drainage.
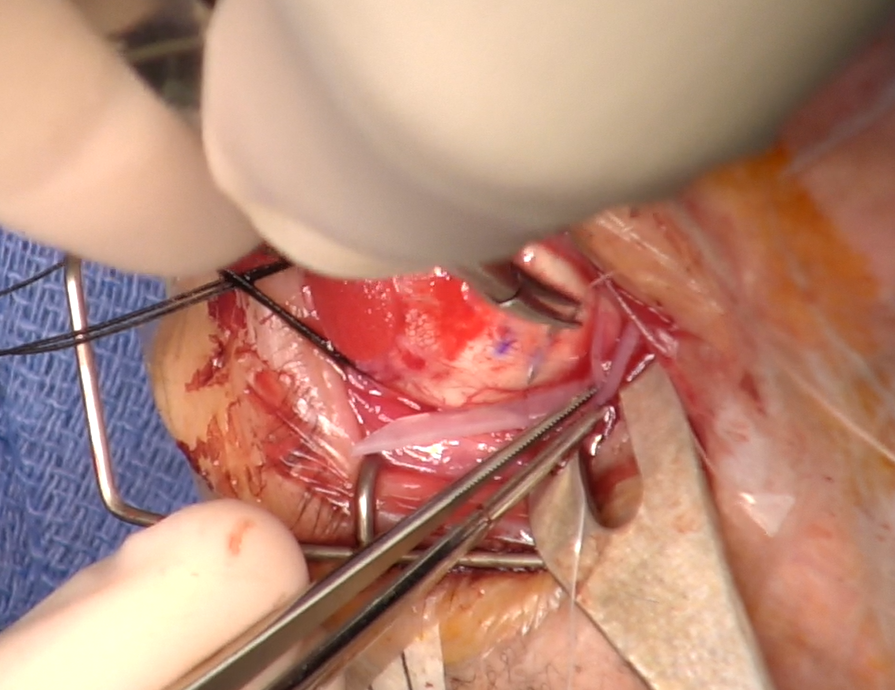
Subretinal fluid drainage - external needle drainage
Other techniques include subretinal entry with a 30g or similar needle without first performing a scleral cut down. This may be done under direct visualization via indirect ophthalmoscopy or chandelier.
Other Techniques Related to Scleral Buckling
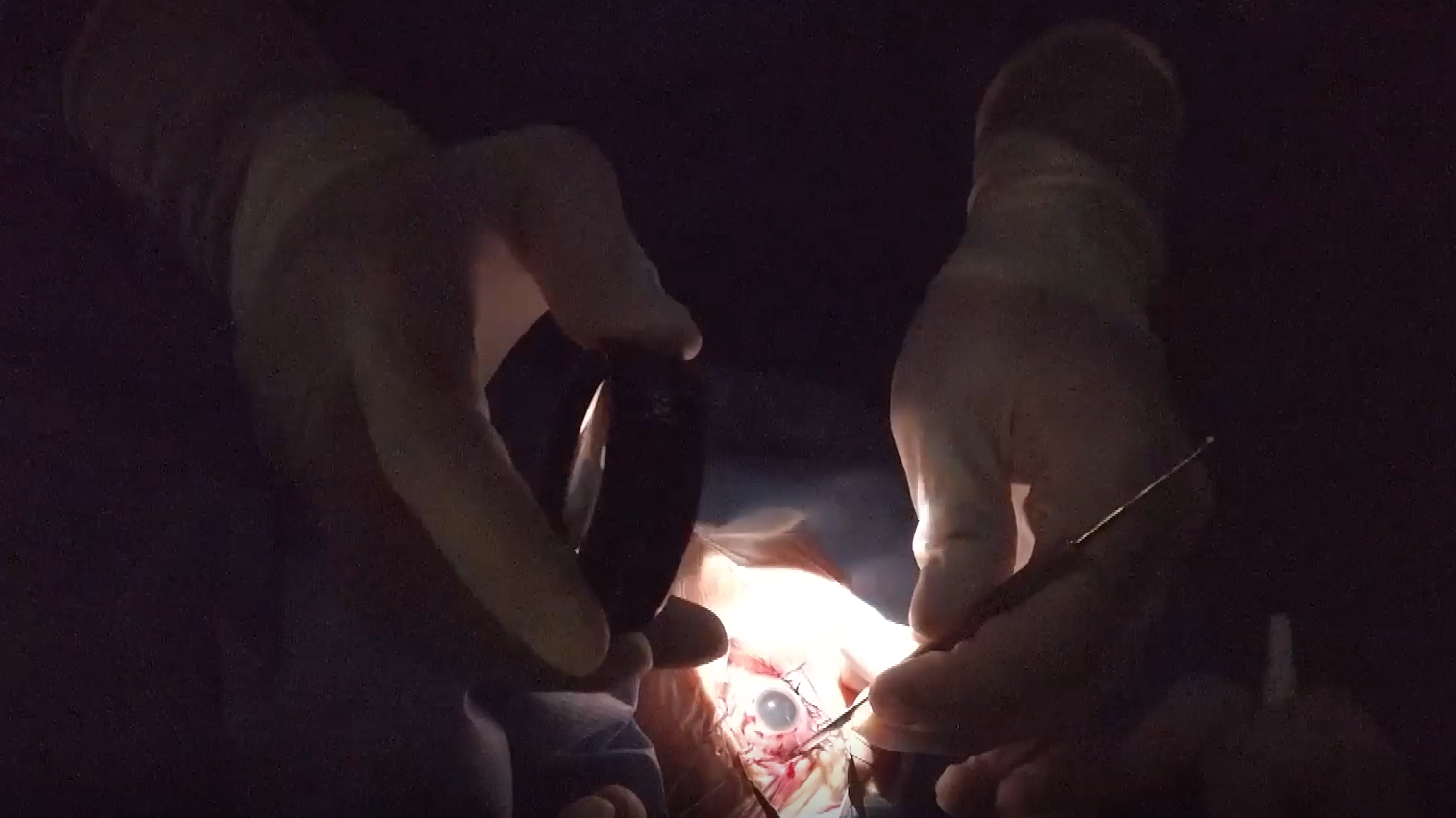
Other Techniques | Scleral buckling under chandelier illumination
Chandelier illumination through the pars plana coupled with a contact or non-contact viewing system and the operating microscope is used to visualize and mark the retinal breaks and otherwise visualize the fundus during steps of the buckling procedure (subretinal fluid drainage, etc). Thus, the remainder of the buckle surgery is also performed under the operating microscope. While the view can be excellent and avoid the hassle of removing and replacing the indirect ophthalmoscope headset (and associated glove changes!), some surgeons believe the benefit of a buckle is never penetrating the globe.
Scleral buckling under chandelier illumination