IMAGE OF THE MONTH: DECEMBER 2021
Asymptomatic unilateral macular lesion


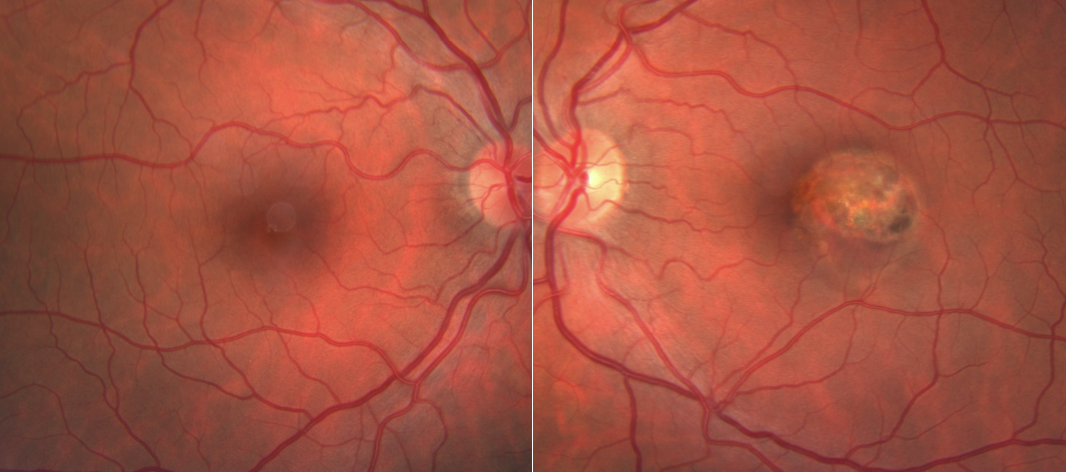
A 40 year-old healthy, asymptomatic female is referred for a “retinal lesion” in the left eye. Her past medical history includes myopia status-post LASIK OU, as well as eczema and alopecia areata treated with steroid creams and intralesional Kenalog. Visual acuity is 20/20 OD and 20/20 OS.
DIAGNOSIS:
Atypical torpedo maculopathy
Discussion:
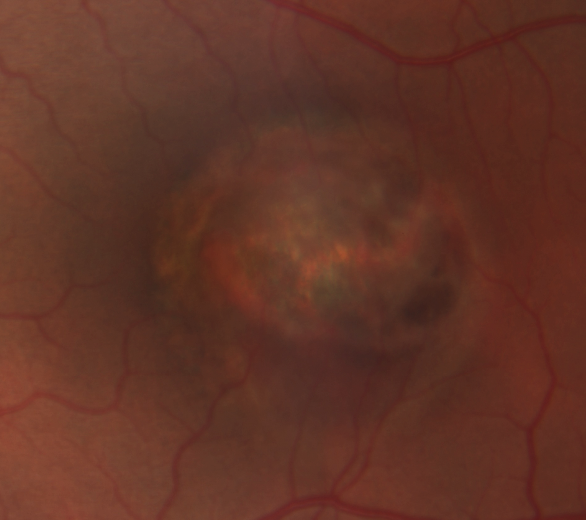
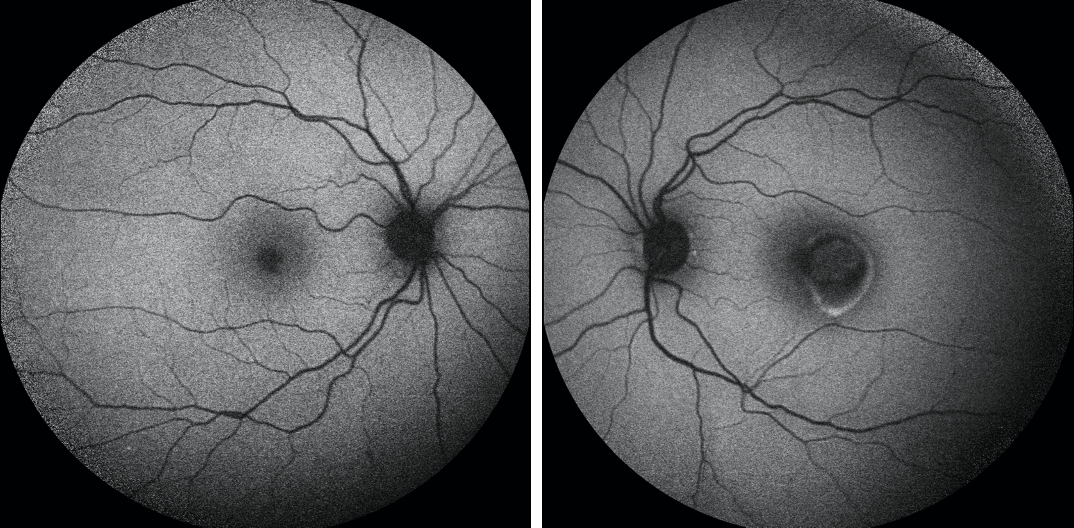
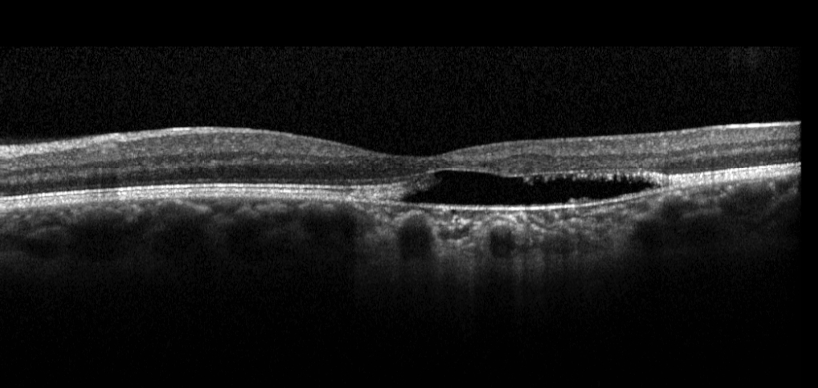
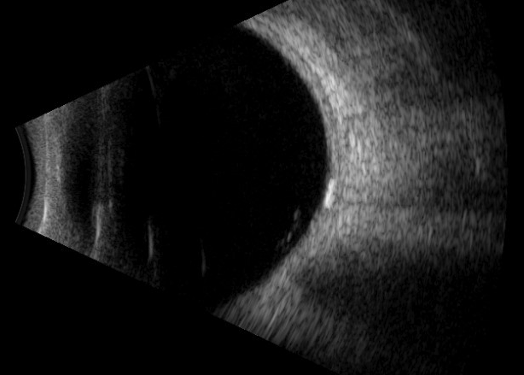
The differential for this macular lesion includes central serous chorioretinopathy (CSCR), choroidal nevus, congenital hypertrophy of the RPE (CHRPE), atypical Best disease, choroidal osteoma, sclerochoroidal calcification, torpedo maculopathy, or RPE hamartoma. The lesion appears variegated in coloration, with areas of hypo- and hyper-pigmentation. On OCT, there is subretinal fluid with disruption of the IS/OS, subretinal deposits of hyperreflective material, and outer retinal excavation. Autofluorescence imaging shows patchy central hypoautofluorescence with a surrounding ovoid ring of hyperautofluorescence. Fluorescein angiography shows late staining of the lesion without leakage, while ultrasonographic B-scan shows a hyperechoic calcified lesion with shadowing adjacent to the optic nerve. Given these findings, a diagnosis of atypical torpedo maculopathy was made.
Torpedo maculopathy is a rare, benign, congenital anomaly of the RPE that is generally non-progressive, though they have been shown to increase in size and occasionally give rise to choroidal neovascularization.1,2,3 These lesions are typically found in the temporal macula and spare the fovea. Torpedo maculopathy can be divided into two subtypes: Type 1 lesions have attenuation of the IS/OS while Type 2 lesions also show outer retinal cavitation with or without inner retinal cavitation.4 The current case is atypical in both its subfoveal location and the finding of hyperechoic calcification on B-scan. However, the patient’s lack of symptoms, as well as OCT and autofluorescence findings, are consistent with torpedo maculopathy. The patient will continue to be monitored for potential growth of the lesion and development of choroidal neovascularization.
References:
1. Sanabria MR, Coco RM, Sanchidrian M. OCT findings in torpedo maculopathy. Retin Cases Brief Rep. 2008;2:109–11.
2. Agarwal A. Gass’ Atlas of macular diseases. 1076. Toronto, Canada: Elsevier Health Sciences; 2011.
3. Jurevic D, Boni C, Barthelmes D, et al. Torpedo maculopathy associated with choroidal neovascularisation. Klin Mon Augenheilkd. 2017;234:508–14.
4. Wong EN, Fraser-Bell S, Hunyor AP, Chen FK. Novel optical coherence tomography classification of torpedo maculopathy. Clin Exp Ophthalmol. 2015 May-Jun;43(4):342-8. doi: 10.1111/ceo.12435. Epub 2014 Nov 7. PMID: 25266677.